THE SCIENCE
HOW IT WORKS
FLOOR MUSCLES AS A CAUSE OF FEMALE SEXUAL
DYSFUNCTION – MECHANISM OF ACTION
- Pelvic floor muscles support the pelvic floor organs, control the continence and play a crucial role in adequate genital arousal
and attainment of orgasm. - Their weakness or deconditioning provide insufficient activity necessary for vaginal friction or blood flow, and therefore inhibit
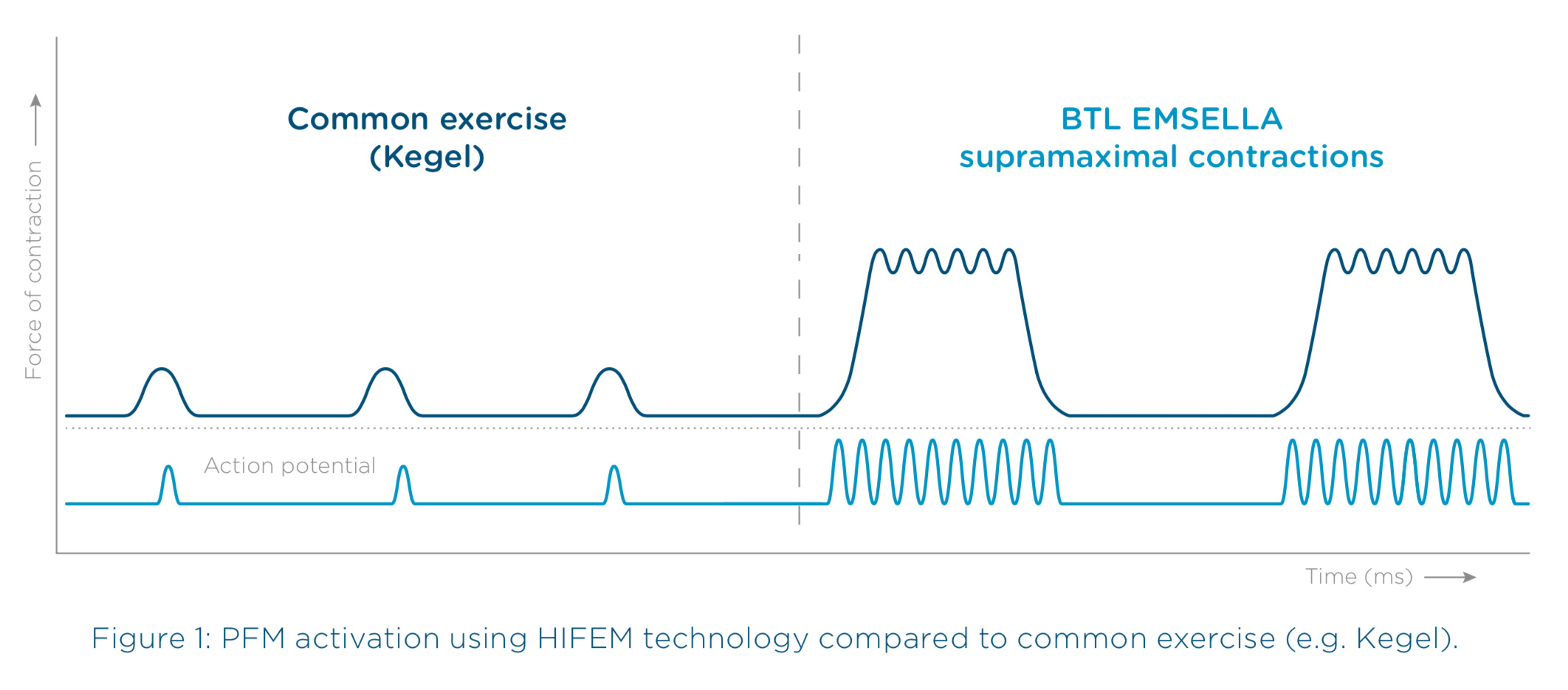
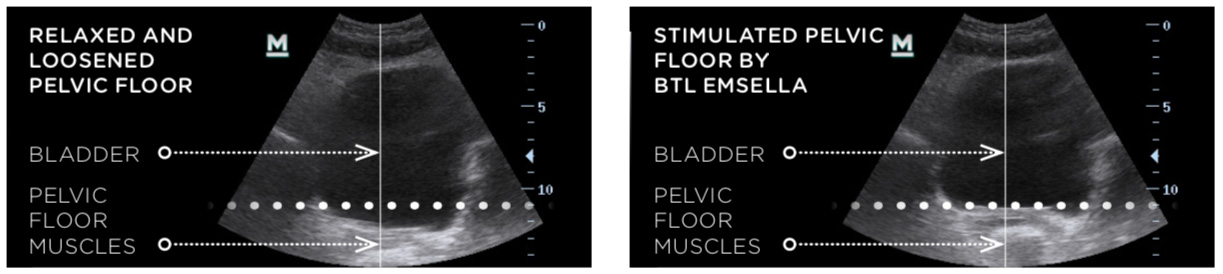
orgasmic potential. - HIFEM therapy key effectiveness is based on focused electromagnetic energy, in-depth penetration, and stimulation
of the entire pelvic floor area. - A single HIFEM session brings thousands of supramaximal pelvic floor muscle contractions, which are extremely important
in muscle stimulation of women with sexual dysfunction.
THE ROLE OF THE PELVIC FLOOR MUSCLES IN SEXUAL LIFE
FEMALE SEXUAL DYSFUNCTION
FSD AND PELVIC FLOOR DISORDER
THE TREATMENT OF PELVIC FLOOR MUSCLES AS A CAUSE OF FSD
HIGH-INTENSITY FOCUSED ELECTROMAGNETIC TECHNOLOGY (HIFEM)

THE ROLE OF THE PELVIC FLOOR MUSCLES IN SEXUAL LIFE
HIFEM THERAPY PROTOCOL
Get Started
Get in touch now

Email Us
info@betterlifenow.co.uk
OFfice (APPOINTMENT ONLY)
Address to go here
Monday – Friday
8am – 5pm
Saturday
10am – 4pm
Sunday
10am – 12pm
References:
1. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The Standardisation of Terminology of Lower Urinary Tract Function. The International Continence Society Committee on Standartisation of Terminology. Scand d Suppl 1998;114:5-19.
2. Almeida FG, Bruschini H, Srougi M.: Urodynamic and clinical evaluation of 91 female patients with urinary incontinence treated with perineal magnetic stimulation: 1-year follow-up. J Urol. 2004 Apr; 171(4), pages 1571-4.
3. Bickford, R., Guidi, M., Fortesque, P. and Swenson, M. (1987). Magnetic stimulation of human peripheral nerve and brain. Neurosurgery, 20(1), pp.110-116.
4. Burri A, Spector T. Recent and lifelong sexual dysfunction in female UK population sample: prevalence and risk factors. J Sex Med 2001; 8:2420.
5. Coletti, D., Teodori, L., Albertini, M., Rocchi, M., Pristerà, A., Fini, M., Molinaro, M. and Adamo, S. (2007). Static magnetic fields enhance skeletal muscle differentiation in vitro by improving myoblast alignment. Cytometry Part A, 71A(10), pp.846-856.
6. First MB, Wakefield JC. Diagnostic criteria as dysfunction indicators: bridging the chasm between the definition of mental disorder and diagnostic criteria for specific disorders. Can J Psychiatry. 2013;58:663–669. [PubMed]
7. Graber B, Kline-Graber G. Female orgasm: role of pubococcygeus muscle. J Clin Psychiatry. 1979;40(8):348-351.
8. Giraldi A, Rellini A, Pfaus JG, Bitzer J, Laan E, Jannini EA, Fugl-Meyer AR. Questionnaires for assessment of female sexual dysfunction: a review and proposal for a standardized screener. J Sex Med. 2011;8:2681–2706. [PubMed]
9. Hayes RD, Bennett CM, Fairley CK, Dennerstein L.: What can prevalence studies tell us about female sexual difficulty and dysfunction? J Sex Med. 2006 Jul;3(4):589-595.
10. Kadri, K. Alami, M. Tahiri, M. 2002, Sexual dysfunction in women: population based epidemiological study. Arch Womens Ment Health , 5,59–63.
11. Kanter G, Rogers RG, Pauls RN, Kammerer-Doak D, Thakar R. A strong pelvic floor is associated with higher rates of sexual activity in women with pelvic floor disorders. Int Urogynecol J. 2015;26(7):991-996. doi:10.1007/s00192-014-2583-7
12. Kao A, Binik YM, Kapuscinski A, Khalifé S. Dyspareunia in postmenopausal women: A critical review. Pain Res Manag. 2008;13(3):243-254.
13. Kegel AH. Sexual functions of the pubococcygeus muscle. West J Surg Obstet Gynecol. 1952;60(10):521-524.
14. Laumann, E. Das, A. Waite, L. 2008. Sexual Dysfunction among Older Adults: Prevalence and Risk Factors from a Nationally Representative U.S.Probability Sample of Men and Women 57–85 Years of Age. J Sex Med, 5, 10, 2300–2311.
15. Laumann, E. Paik, A. Rosen, R.1999. Sexual Dysfunction in the United States Prevalence and Predictors. JAMA, 2, 81:537-544.
16. Laumann, EO. Nicolosi, A. Glasser, DB. Paik, A. Gingell, C. Moreira, E. Wang, T. 2005. Sexual problems among women and men aged 40–80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. International Journal of Impotence Research,17, 39–57.
17. Lindau, s. Schumm, P. Laumann, O. Levinson, W. O’Muircheartaigh, C. Waite, L. 2007. A Study of Sexuality and Health among Older Adults in the United States.. N Engl J Med, 357, 22-34.
18. Ma Y, Qin H. Pelvic floor muscle exercises may improve female sexual function. Medical hypotheses. 2008;72:223. doi:10.1016/j.mehy.2008.09.026
19. McCabe MP, Sharlip ID, Lewis R, et al. Proceedings from the 4th International Consultation on Sexual Medicine committee 1: current definitions, classification and epidemiology of sexual dysfunction in women and men. 2015.
20. Ostrovidov, S., Hosseini, V., Ahadian, S., Fujie, T., Parthiban, S., Ramalingam, M., Bae, H., Kaji, H. and Khademhosseini, A. (2014). Skeletal Muscle Tissue Engineering: Methods to Form Skeletal Myotubes and Their Applications. Tissue Engineering Part B: Reviews, 20(5), pp.403-436.
21. Reider B. Role of Pelvic Floor Muscles in Female Orgasmic Response. Journal of Women ́s Health, Issues and Care. 2016;2016. doi:10.4172/2325-9795.1000250
22. Rogers RG. Sexual function in women with pelvic floor disorders. Can Urol Assoc J. 2013;7(9-10 Suppl 4):S199-S201. doi:10.5489/cuaj.1625
23. Shafik A. Vagino-levator reflex: description of a reflex and its role in sexual performance. European Journal of Obstetrics & Gynecology and Reproductive Biology. 1995;60(2):161-164. doi:10.1016/0028-2243(95)02095-A
24. Shafik A. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(6):361-376.
25. Smith AMA, Lyons A, Ferris JA, et al. Incidence and persistence/recurrence of women’s sexual difficulties: findings from the Australian Longitudinal Study of Health and Relationships. J Sex Marital Ther 2012; 38:378
26. Stölting, M., Arnold, A., Haralampieva, D., Handschin, C., Sulser, T. and Eberli, D. (2016). Magnetic stimulation supports muscle and nerve regeneration after trauma in mice. Muscle & Nerve, 53(4), pp.598-607.
27. Wallis, M., Davies, E., Thalib, L. and Griffiths, S. (2011). Pelvic Static Magnetic Stimulation to Control Urinary Incontinence in Older Women: A Randomized Controlled Trial. Clinical Medicine & Research, 10(1), pp.7-14.